Value-based care has been a breakthrough idea for payers. But to many physicians, it might seem like the vampire that just won’t die.
Yes, it’s designed to lower costs in the long run, a goal most of us can support. But there’s always a fear that it might not align with optimum patient care … and can put a significant burden on your practice.
Still, value-based care seems to be creeping into more contracts as payers, particularly the government, work to get costs under control. So, the question arises: Are there ways to leverage it for the good of your practice? Here are 3 strategies to consider.
1. Amp Up Your Patient Satisfaction Rates
The shift toward value-based care has put a stronger emphasis on patient satisfaction rates. In that capacity, you’ve always been ready to deliver excellent medical care. But maybe you could look at some extra details that are part of the care experience at your office.
For example, you might see opportunities to:
- Improve your scheduling system
- Make your billing statements easier to understand
- Increase your number of follow-up calls and appointment reminders
You also might consider providing financial counseling to patients, or referrals to payment assistance programs, if you’re not already doing so.
Value-adds like these can boost patient satisfaction rates and improve health outcomes in the process.
2. Launch Quality Improvement Projects
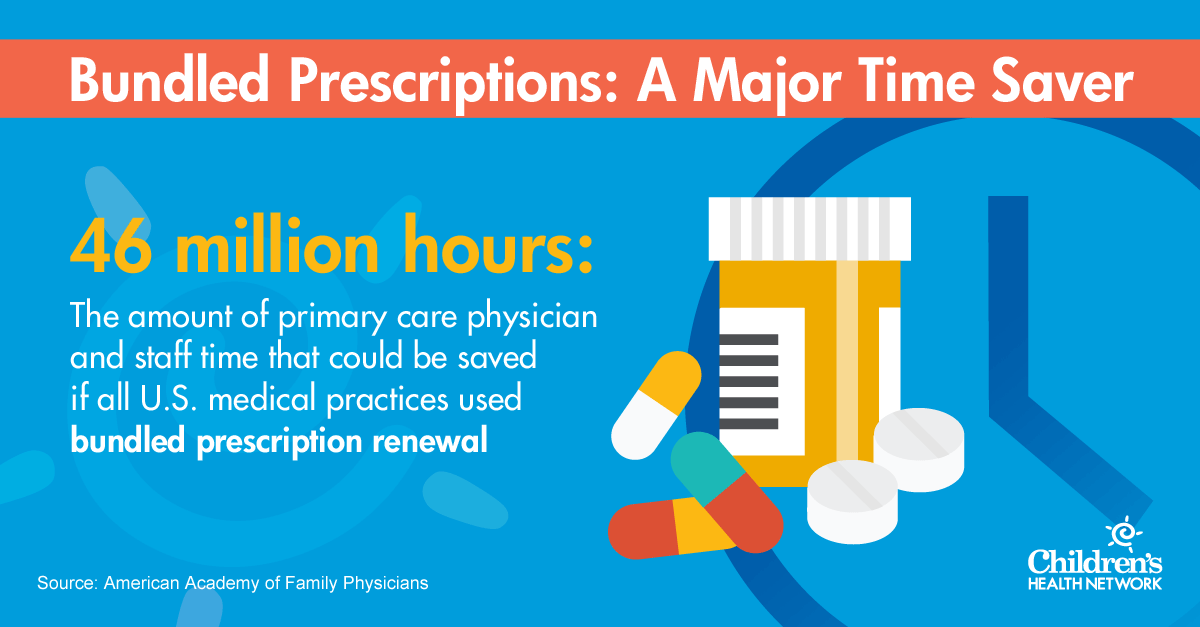
It’s an old formula: Prevention saves money. If your reimbursements will be tied to your patients’ long-term health, maybe it’s time to take a look at some new quality initiatives in your practice.
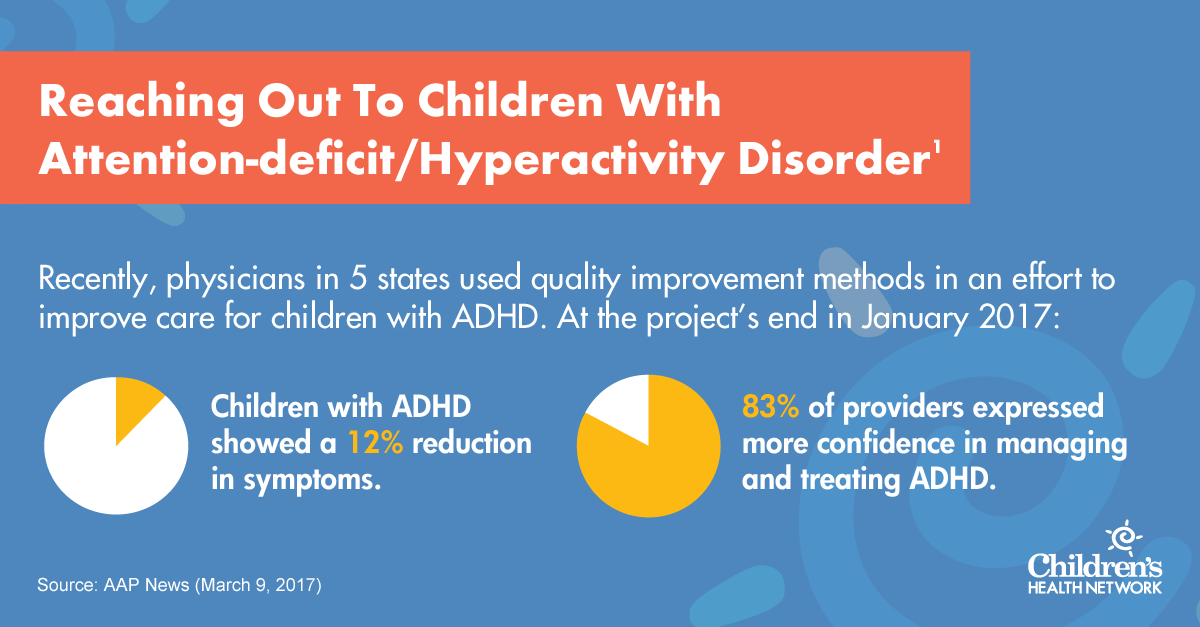
Your quality improvement projects can provide valuable data to payers in the value-based care arena and tie into parallel projects, such as complying with HEDIS quality measures.
3. Make A Stronger Impact On Population Health
It’s no secret that payers have taken a stronger interest in population health management as they move toward value-based care. This gives physicians an opportunity to look more broadly at their patient populations — for example, children with chronic conditions like asthma or diabetes.
To “move the needle” toward better health for these patients, the Health Information and Management Systems Society (HIMSS) suggests three keys to a successful population health management program2:
- Data analytics
- Technology adoption
- The inclusion of the patient as a partner
In particular, consider new technology that provides real-time data and predictive analytics. These tools can drive clinical decisions that better support your patient populations, HIMSS notes. Contact a health information technology consultant to discuss how to implement tools like these with your EMR and workflow.
When your at-risk patient populations start to show better numbers — fewer hospitalizations, more days without asthma attacks, lower blood sugar — you’ll not only create grateful parents. You might also make value-based care contracts easier to manage over time.
Share this article with a colleague who is implementing value-based care contracts into his practice.